Regenerative medicine is one of the fastest-growing fields in veterinary science, with new research papers published every day. As a busy mom of two, I’ll admit I don’t always have the time to keep up with all of it—and I know many veterinary professionals are in the same boat.
I’m Dr. Adrienne Wright, Site Leader and VP of Science and Commercialization at Ardent Animal Health. Life can get busy and overwhelming, and after a long day in the clinic, most of us aren’t reaching for 16 pages of dense scientific data to relax. That’s why I created this podcast: short, 10–15 minute episodes where I read the papers, break them down, and give you the key points you need to stay current.
Listen anywhere you get your podcasts…
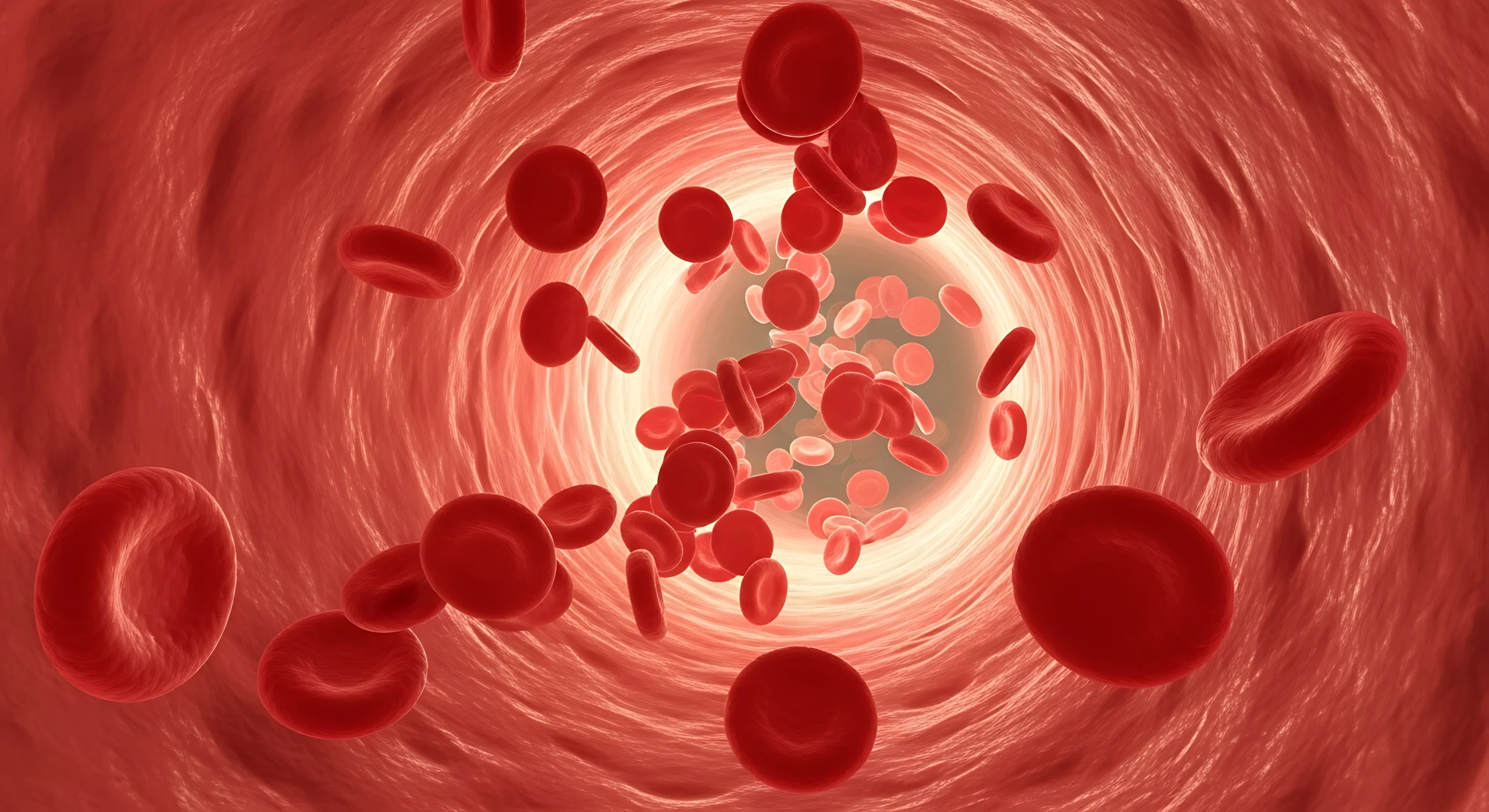
Why Platelet-Rich Plasma (PRP)?
For our first episode, I wanted to look at platelet-rich plasma (PRP). Two veterinarians recently emailed me asking whether PRP has antimicrobial properties. Honestly, I’d never really considered it before—but if it does, that would be another big advantage on top of its known uses for joint injections. It might also explain why we rarely see complications after intra-articular PRP use.
PRP is also a game changer for wound healing. I’ve always thought of it in that context, but not necessarily for its antimicrobial potential. That led me to a paper from a group in Portugal on wound management in dogs using platelet-rich fibrin (PRF).
PRF is actually part of the Ardent PRP system—the gel clot that forms after centrifugation when platelets are concentrated. For injection, we add solution G and use the liquid fraction. For PRF applications, we use the clot itself.
Study Overview
The paper described eight dogs, ages 7 months to 9 years, with a variety of wounds:
- Dog bite
- Subcutaneous ruptured abscess
- Traumatic chronic wound
- Ulcerative lesion post-surgery
- Myiasis infection
- Laceration
Five were female, three male. Most were already on conventional medications. PRF clots were applied directly to the wounds.
Treatment schedules varied:
- In three cases, dogs received two treatments in the first week, then once weekly until closure.
- In five cases, they received two treatments per week for two weeks, then once weekly until closure.
No topical antibiotics, antiseptics, or wound-healing drugs were used during the study.
Results
- No adverse reactions reported—no allergies, rash, fever, or other side effects.
- All treatments produced notable granulation tissue formation with no signs of infection or necrosis.
- Complete wound closure in 7 of 8 cases occurred in a median of 31 days (range: 13–42 days).
- Dry crust formation was seen in 7 cases; hair regrowth occurred in all.
- Recurrence was rare—only 2 cases, both associated with pre-existing neoplastic lesions.
A positive correlation was found between initial wound size and healing duration, as well as the number of PRF clots required. Larger wounds took longer to heal and needed more material.
Interestingly, the number of clinic visits for bandage changes was reduced with PRF compared to conventional wound therapy—something to consider when discussing costs with clients.
Takeaways
This case series—though uncontrolled—suggests PRF can:
- Trigger local healing processes
- Promote rapid wound contraction, especially in the first two weeks
- Reduce the need for surgical intervention
- Lower the frequency of bandage changes and clinic visits
- Provide a viable alternative or adjunct to conventional wound therapy
While this is a small sample, it reinforces what many in the field already believe: PRP and PRF should be tools in every veterinarian’s wound care toolbox.
Your Turn
What do you think about the wound-healing potential of PRP? Do you believe it has antimicrobial properties?
You can read the full study and share your thoughts with me at adrienne@ardentanimalhealth.com.
For more episodes, stay tuned to Sit. Stay. Learn.—and remember, I’ll keep doing the reading so you can keep doing what you do best: caring for animals.