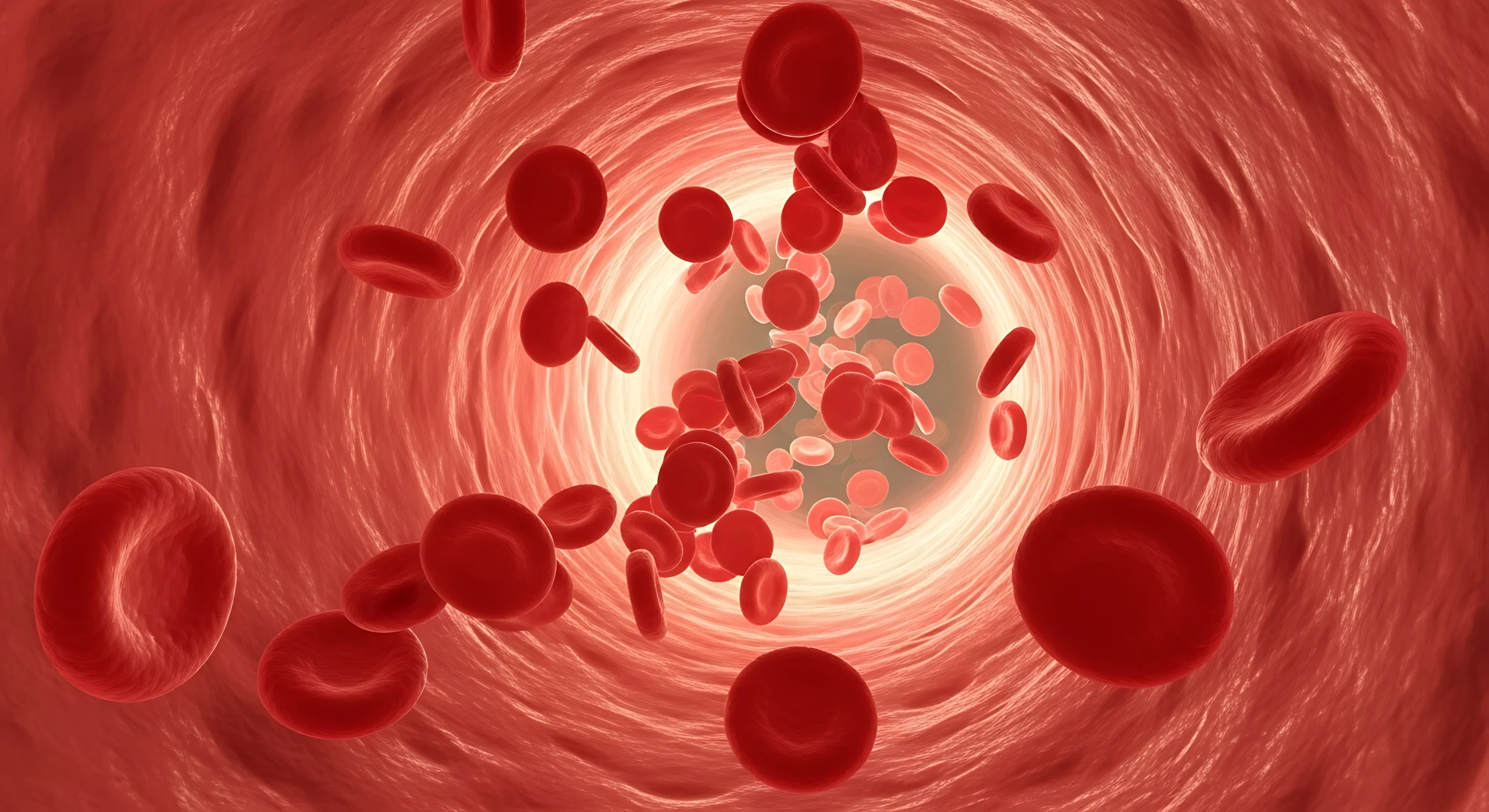
This week’s episode highlights an editorial published in Biomedicines in 2023 titled “Red Blood Cells in Platelet-Rich Plasma: Avoid If at All Possible” by Gupta, Maffulli, and Jain.
While not a traditional research study, the piece brings forward important considerations about how red blood cell (RBC) contamination may influence PRP quality and clinical outcomes.
Listen anywhere you get your podcasts…
Why This Matters
PRP is straightforward to prepare in principle, but real-life blood draws can be challenging. If hemolysis occurs, the plasma layer may appear red after centrifugation, raising the question of whether the sample is still usable. Clinics frequently weigh the ideal scientific answer—a clean redraw—against practical factors such as patient comfort, the need for additional tubes, travel constraints for owners, and whether another draw is feasible at all.
Understanding what hemolysis does biologically helps guide those decisions.
Study Overview
The authors of the editorial point out that PRP systems vary widely in how they separate platelets, leukocytes, and RBCs. Because formulations differ, outcomes reported across studies can be inconsistent. They emphasize that RBC contamination is a key variable contributing to this variability and deserves more attention when preparing PRP.
Findings From the Literature
The editorial summarizes several studies showing that when RBCs break down, they release hemoglobin, iron, and hemin—components that can activate inflammatory pathways, create oxidative stress, and contribute to chondrocyte and synovial cell damage. In both in vitro work and animal models, exposure to blood or RBC concentrates has been linked to cell death, impaired cartilage turnover, and long-term degenerative changes.
Some evidence also suggests that mixing RBCs with PRP may trigger eryptosis and cytokine release, potentially reducing the therapeutic intent of the injection.
Overall, these findings support the authors’ recommendation to minimize RBCs in PRP whenever possible.
Final Thoughts
Although there are no direct clinical studies comparing RBC-rich to RBC-poor PRP, the available evidence suggests that hemolysis may reduce the effectiveness of PRP and increase inflammatory risk, especially in joint applications. When feasible and safe for the patient, a redraw is still the preferred approach.
That said, each case is unique. Many decisions depend on patient well-being, logistics, and the resources available at the moment. Understanding the science behind hemolysis helps clinicians make more informed choices when navigating those gray areas.
If you are interested in the full study, download it here. For questions or further discussion, feel free to reach out to adrienne@ardentanimalhealth.com. If your practice has experience managing hemolyzed PRP samples, your insights are welcome.