Today’s Paper: PRP for Prostatic Cysts
This week, I reviewed a case study sent to me by our own technical services veterinarian, Dr. Larry Snyder. If you’ve never had the chance to talk with Dr. Snyder, you should—he’s got over 20 years of regenerative medicine experience and a passion for helping vets think through tough cases.
The paper itself looked at platelet-rich plasma (PRP) for the treatment of prostatic cysts in dogs. It comes from researchers in Italy and was published in The Canadian Journal of Veterinary Research in 2018.
Listen anywhere you get your podcasts…
Why This Matters
Prostate abnormalities are common in older male dogs—especially medium to large breeds—where incidence can be as high as 80% after age 5.
- Prostatic cysts are seen in ~14% of large-breed males, and nearly half of those carry bacterial contamination, which can transfer to semen. That’s a big issue for AI programs.
- The biggest complication is progression into abscesses, which can be life-threatening.
- Current treatment options—like chemical castration, orchiectomy, alcohol sclerotherapy, or surgical reduction—each come with their own drawbacks. Recurrence rates are high, procedures can be invasive, and none of the approaches are consistently effective or complication-free.
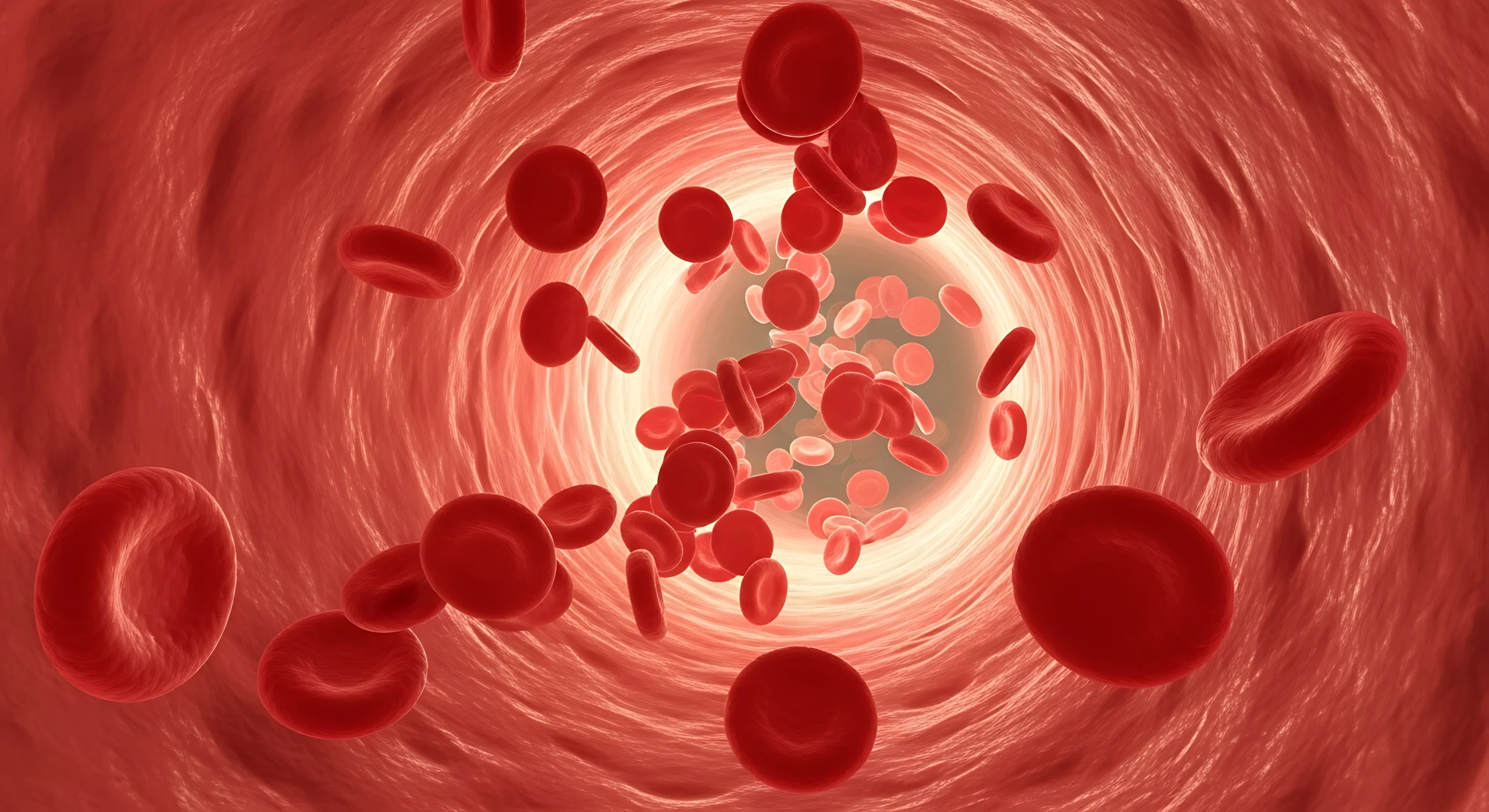
Against that backdrop, PRP may sound like an odd choice. But its biological activity—growth factors, cytokines, and bioactive compounds released during platelet degranulation—makes it a compelling candidate for modulating inflammation and promoting tissue repair. At the time of this study, there was no literature on PRP for prostatic cysts, which makes this trial both unique and bold.
Study Design
- Subjects: 10 mixed-breed adult male dogs
- Ages: 4–7 years (median 5.5)
- Weights: 22–35 kg (median 25.9)
- Intervention: single PRP injection following ultrasound-guided drainage
- Follow-up: days 6, 12, 24, and 60
A nice detail here: in dogs with multiple cysts, only one was treated with PRP, while the others acted as controls. For a case study, a sample of 10 dogs plus internal controls is actually quite robust.
The PRP was prepared autologously. What stood out to me is that the researchers adjusted PRP volume after capturing a platelet count to hit a 3–5x concentration, but I didn’t see evidence of platelet activation in their protocol. Without activation, you risk losing some therapeutic potential since growth factors may not be fully released.
By comparison, using Ardent’s kit would streamline this—draw 9–36 mL of whole blood, process it in 45 minutes, and you’ve got 3–4 mL of PRP concentrated, activated, and ready to deliver.
Results
- Immediately after injection: ultrasound showed cysts were hypoechoic with vague margins.
- Day 6: hypoechoic appearance maintained, cysts still visible.
- Day 12: cyst volume reduced by ~50%.
- Days 24 & 60: cysts were no longer detectable by ultrasound.
An interesting note: one dog in the study was euthanized a year later due to an unrelated oral tumor. Necropsy showed that the injected cyst had collapsed with poor secretions, while untreated cysts still showed thick connective tissue and secretory epithelium.
No adverse events were reported. All therapies were well tolerated.
Why It’s Exciting
For me, the most impressive part is that every dog responded positively. By 60 days, treated cysts had essentially disappeared, while untreated cysts persisted with signs of inflammation.
The authors hypothesized that PRP helped by reducing inflammation, allowing tissue balance to reset and cystic fluid to be reabsorbed. That fits well with what we already know about PRP’s anti-inflammatory and regenerative roles.
Of course, it’s still a case study with a limited sample size. Larger trials with more controls would be needed before making PRP a frontline option. But the results are encouraging—especially since no other therapy for prostatic cysts is both effective and low-risk.
Final Thoughts
This study suggests that PRP, combined with ultrasound-guided drainage, could be a safe and innovative alternative for treating prostatic cysts in dogs.
It’s rare to see a case series where all subjects benefit so clearly. While more work needs to be done, this paper makes a strong case for adding PRP to the toolbox for managing prostatic disease.
What do you think—could PRP become a game-changer for prostatic cysts?
You can read the full study and email me at adrienne@ardentanimalhealth.com.