This week, we’re taking a slightly different path. Most of the studies we review focus on veterinary applications, but this one looks at a human pilot study that offers meaningful insights for how we approach chronic kidney disease (CKD) in pets.
Listen anywhere you get your podcasts…
Why This Matters
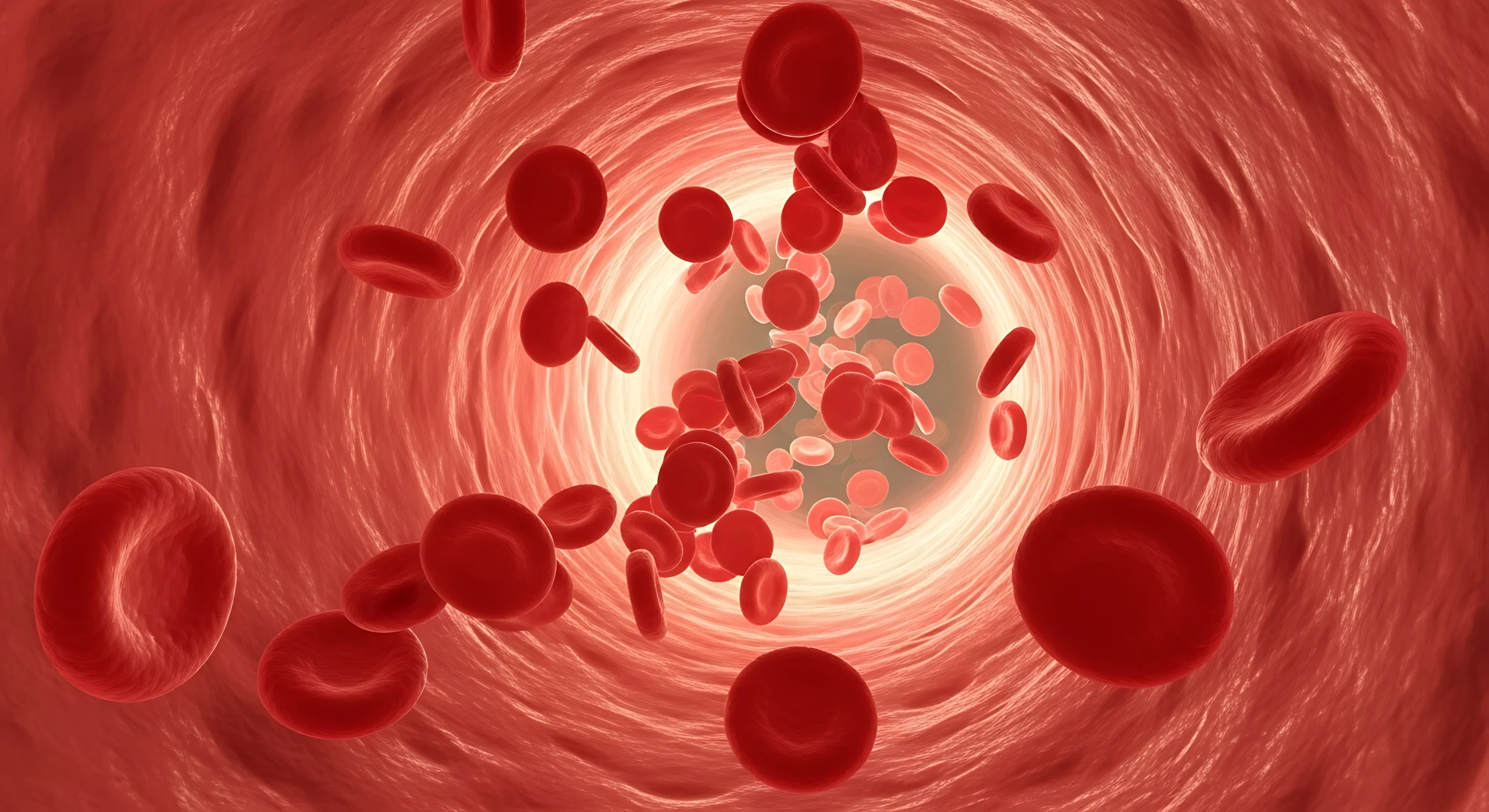
TGR is a go-to procedure for dogs with patellar luxation, but recovery can be complicated by inflammation and Chronic kidney disease is a long-term, progressive condition that affects both humans and animals. It’s one of the most common causes of illness in older dogs and cats—impacting roughly 10% of senior dogs and up to 50% of cats over 15 years old.
While current treatments can slow the progression of CKD, they can’t reverse it. This is where mesenchymal stromal cells (MSCs) have captured attention. Known for their anti-inflammatory, regenerative, and immune-modulating properties, MSCs have shown promise in protecting kidney tissue and improving overall function.
At Ardent, we’ve seen similar benefits in cats treated with stem cells—improved appetite, energy, and weight stability—even when bloodwork changes are modest.
Study Overview
- Participants: 7 adults were enrolled (6 completed the study). Average age: 42 years.
- Condition: All had moderate CKD, with average creatinine levels of 2.22 mg/dL.
- Treatment: A single intravenous infusion of autologous adipose-derived MSCs (1 million cells/kg in 120 mL of LRS, given over 30–40 minutes).
- Design: Each patient served as their own control, comparing kidney function and symptoms during the 12 months before treatment versus the 12 months after.
Results
The treatment was well tolerated, with no infusion-related adverse effects. Laboratory values—including liver, coagulation, and metabolic markers—remained stable.
Proteinuria, a key marker of kidney damage, decreased in nearly every patient after MSC therapy. Even patients with more advanced kidney damage showed slower disease progression compared to the year before treatment.
While overall eGFR changes were not statistically significant, five of six patients experienced reductions in creatinine (ranging from 7.5% to 49%). Those with less inflammatory disease appeared to stabilize more effectively.
Key Findings
- Safe and feasible: The single IV dose was well tolerated in every participant.
- Proteinuria improvement: A consistent finding across nearly all patients.
- Clinical relevance: The improvements in kidney stability and inflammation mirror results seen in some veterinary cases.
- Practicality: Adipose tissue offers an accessible, high-yield MSC source compared to bone marrow, which may be less effective in CKD patients.
Final Thoughts
This pilot study reinforces the potential of adipose-derived MSCs as a supportive therapy for CKD—both in people and animals. While more controlled trials are needed, these early results highlight a promising, well-tolerated treatment that aligns with what many veterinary practitioners already observe in the field: even modest physiologic changes can translate to significant improvements in quality of life.
Could stem cell therapy become a more standard part of CKD management for our veterinary patients? Studies like this one bring us a step closer to answering that question.
For more discussion and insights, listen to this episode of Sit. Stay. Learn. or contact adrienne@ardentanimalhealth.com.
If you’ve used PRP or cell therapy in a TGR case, I’d love to hear your results. You can reach me at adrienne@ardentanimalhealth.com.